Tracking the Recovery of Breast Cancer Care Following the COVID-19 Slowdown

Widespread awareness of the importance of preventive screening and early intervention has made breast cancer one of the great public health success stories. Between 1989 and 2017, the breast cancer death rate in the US declined 40%, helping to drive the overall cancer death rate to its largest one-year drop between 2016 and 2017.
This achievement owes a great deal to the mammogram. Studies show that for women of all ages and at average risk, breast cancer screening is associated with a reduction in breast cancer mortality of approximately 20%. Accordingly, the American Cancer Society recommends that all women begin having yearly mammograms by age 45, switch to a biennial frequency at age 55, and continue screening as long as they are in good health and expected to live 10 more years or longer.
But what happens when a huge slice of the population suddenly stops having mammograms? That’s exactly what happened in March through May of 2020 as the COVID-19 pandemic caused the majority of the US population to put preventive care on hold. This was driven both by the pause in “non-emergency” care and by patients’ fear of contracting COVID-19 inside health facilities. How the healthcare system and the American public address the months-long gap in care will have a significant impact on our country’s ability to continue to improve breast cancer outcomes. Based on current patient behaviors, however, we still have a long way to go to close that gap.
Tracking the Ripple Effects of COVID-19 on Breast Cancer Care
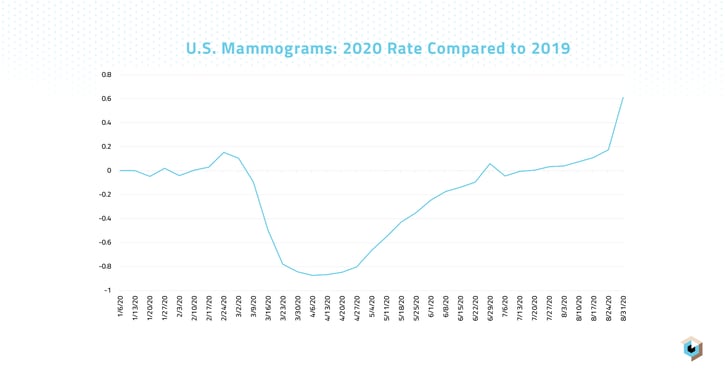
To get a better understanding of how COVID-19 has affected breast cancer care, we analyzed our Healthcare Map of real-world patient encounters to track trends in mammogram volume, new breast cancer diagnoses, and breast cancer surgeries throughout 2020 and compared them year over year to the rates for the same procedures in 2019. Across the board, the data show a sharp decline in breast cancer care throughout the months of March, April, and May of 2020. More recently, volumes have started to climb, but the pace of increase remains far below the pace of decline we saw during the height of the pandemic.
Looking at mammogram volumes, for example, we saw the overall number of screenings start to fall sharply starting the week of March 9, 2020, reaching its lowest point during the weeks of April 6 and April 13, 2020, when volumes were down 87% versus 2019 totals. Weekly mammogram volumes continued to stay significantly suppressed versus 2019 totals throughout April, May, and June, though the magnitude of decline became smaller with each month. By the week of June 22, 2020, the weekly mammogram rate had fallen to just 9% below the rate seen in the same week of 2019. Starting on July 27, 2020, mammogram rates began to steadily surpass those of 2019, likely representing patients “catching up” with mammogram appointments that had been deferred earlier in the pandemic.
The trendline followed a similar path for new breast cancer diagnoses, which were down 59% versus 2019 volumes at their lowest point, the week of April 20, 2020. Unlike mammogram volumes, however, which started to consistently make up for lost ground starting in July, weekly diagnosis rates did not start to surpass those of 2019 until the week of August 31, 2020, when diagnoses were 17% higher than the previous year. This likely is an indication that there are many more cases that emerged during the pandemic, cases that have still not been diagnosed.
This scenario is loosely supported by our data showing that even surgeries following breast cancer diagnoses were put on hold during the pandemic. The total number of breast cancer surgeries was down 40% versus last year at its low point, the week of April 20, 2020, and it continued to stay suppressed by double-digit percentages through the week of August 3, 2020. The long-term effects of these missed surgeries has yet to be determined.
Awareness Efforts More Essential Than Ever
October is Breast Cancer Awareness Month. Perhaps no October in the history of this campaign has been more important for spreading the word about the need for preventive screening. Unfortunately, even Breast Cancer Awareness Month has been overshadowed by COVID-19. The annual rite of fundraising walks, special events, and pinkwashed sports teams has been strained by the pandemic.
Patient outreach and advocacy will be critical to offsetting the sharp declines in breast cancer care. Providers, payers, and public health officials need to be aware of the stark gap in care that was created by the COVID-19 pandemic and work together to encourage women to close that gap as quickly as possible.
It is also important to recognize that the trend we’re seeing in breast cancer care during the pandemic is part of a much larger trend of deferred or delayed care for everything from childhood immunizations to colonoscopies to routine cholesterol tests. It is essential that we continue to measure these trends to understand the full impact of these gaps in care on national public health.







