Telemedicine Surge Reveals Large Geographic Gaps in Utilization

By most accounts, telemedicine was one of the bright spots in the COVID-19 crisis. The technology helped ease the burden on the healthcare system by allowing patients with non-urgent conditions to receive care via phone and video and it was the first vital line of triage as COVID-19 cases started to spread nationwide. Accordingly, the number of healthcare providers offering telemedicine care climbed from just 3% prior to COVID-19 to 34% nationwide by June 24, 2020.
On the surface, these numbers are encouraging. Telemedicine has been lauded for years as an important tool to close gaps in care, providing access to the healthcare system for people with mobility challenges, those in rural areas, and so-called “medical deserts” who live many miles from the closest provider. The technology also introduces the potential for efficiency gains on the provider side.
Within the stratospheric growth over the last few months, however, there has been an uneven rate of adoption in different parts of the country. A gap of 17 percentage points separates the states with the largest portion of providers offering telemedicine during the pandemic (Vermont and Rhode Island) and the states with the lowest level of adoption (Missouri and Montana).
State-by-State Telehealth Utilization By the Numbers
We recently explored this phenomenon using our Healthcare Map to evaluate the patient journeys associated with 320 million individuals in the U.S., tracking the total number of telehealth encounters on a statewide basis, both pre-pandemic and during the pandemic. The pre-pandemic era was defined as March 1, 2019 to February 29, 2020, while the pandemic era was defined as March 1, 2020 to June 23, 2020.
Our preliminary analysis shows that on a nationwide basis as stated above, the total number of providers offering telemedicine climbed from 3% during the pre-pandemic period to 34% during the months following shelter-in-place orders. That translates to roughly 23 telemedicine-enabled providers for every 100,000 patients nationally pre-COVID-19 and 161 telemedicine-enabled providers for every 100,000 patients nationally during the COVID-19 pandemic.
While the overall utilization of telemedicine grew considerably during the pandemic, that growth was uneven on a state-by-state basis. Vermont and Rhode Island had the largest percentage of providers offering telemedicine during the pandemic, with 44% of the state’s providers delivering virtual care during the pandemic era. This represented a 10.5x increase in the number of telemedicine-enabled providers in Vermont and 18.6x more providers offering telemedicine in Rhode Island. By comparison, Missouri and Montana had the lowest adoption rate among providers with just 27% of providers offering telemedicine during the pandemic era.
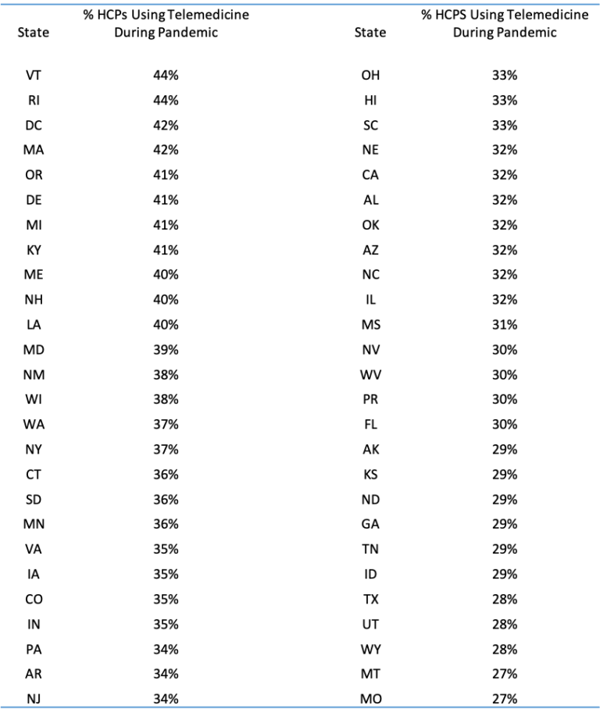
The states with the steepest rate of telemedicine adoption during the pandemic were Massachusetts, which saw its proportion of providers offering telemedicine increase 19.2x during the pandemic. Followed closely by Rhode Island (18.6x), New Hampshire (16.6x), and Connecticut (13.9x).
New York saw its total number of providers offering telemedicine services increase 11.6x during the pandemic, bringing its total adoption to just above average (37%). California had the smallest increase at just 2.7x, but it is worth noting it had the largest proportion of providers offering telemedicine prior to the pandemic (8%).
Tracking Gaps in Care
The data in our analysis suggests that a critical mass of patients and providers have indeed embraced telemedicine during the pandemic and that may be enough of a catalyst to shape the future growth trajectory of the technology. The uptick in adoption is likely explained by the combined efforts by both providers and patients to avoid exposure, as well as an increase in payment to reimburse for telehealth services. Recent CMS guidelines have changed to allow billing for telehealth visits which likely contributed to the increase in claims. It is possible that some providers were utilizing telemedicine prior to the pandemic but were not seen in our data because they were not incentivized to bill for it.
However, the geographic gaps in adoption raise a number of questions. While the effects of the pandemic have been felt unevenly throughout the country, the states showing the largest growth in telemedicine do not correlate evenly with the states showing the largest or smallest rates of infection. There is also no obvious linkage between population density, urban vs. rural, or region of the U.S. Possible exogenous influences on the data could include variation in health plan coverage in different states, patient access to technology, and even age-based demographic factors.
While the topic certainly requires a great deal more research, what these early findings do tell us is that — within the nationwide surge in telemedicine volume — utilization rates have been uneven in the U.S. That’s a critical trend that will be important to monitor as telemedicine becomes more commonplace in the U.S. healthcare system.







