Race & Disparities in Care: Emergency and Inpatient Treatment in Chronic Diseases

Chronic disease discriminates. Responsible for more deaths and higher overall healthcare costs than any other cause, chronic conditions such as heart disease, cancer, and diabetes disproportionately affect populations of color, older adults, and those with lower incomes. While this trend has been documented for years, the problem persists, creating one of the most significant public health challenges of our time.
Deconstructing how exactly these barriers present themselves and how to overcome them is trickier business. For decades, studies have highlighted this problem, but much of this research was based on incomplete EHR data or data from one institution. Without a single, complete source of data, stakeholders throughout the industry have struggled to change the pattern and improve health equity. Often, this lack of progress comes down to an incomplete understanding of the problem, which is exacerbated by disparate datasets that are incapable of informing meaningful patient outreach and policy implications.
Today, it is possible to break down many of the data silos that have historically limited visibility into the experiences behind these trends. By digging deep into real-world patient journeys of people in these underserved segments of the population, we can better understand the behavioral, sociodemographic, and clinical factors driving disparities in care.
Komodo Health has started that process with a new analysis, published today, that tracks healthcare utilization trends across racial groups in patients with three specific chronic diseases: Alzheimer‘s disease, chronic obstructive pulmonary disease (COPD), and osteoporosis. Using insights from Komodo’s Healthcare Map™, the analysis spotlights variations in the healthcare experiences of patients representing different demographic groups.
Following are the key findings from our report:
Patients of color visited the emergency room and were admitted as inpatients more often than White patients, suggesting more frequent and more serious complications of their chronic conditions. For instance, patients of color with Alzheimer’s disease experienced 20% more emergency room visits and 54% more inpatient admissions compared with White patients. COPD patients of color visited the ER 39% more than White patients, and were admitted to the hospital 43% more often.
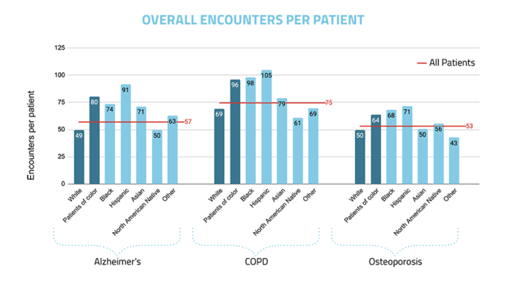
Similarly, the report also found that overall healthcare utilization was higher among populations of color with Alzheimer’s, COPD, and osteoporosis compared with the White population with these conditions. The Hispanic population, in particular, demonstrated high levels of healthcare utilization with an average of 91 encounters per patient for Alzheimer’s over a two-year period, 105 encounters per patient for COPD, and 71 encounters per patient for osteoporosis in the same timeframe. In contrast, the White population averaged 49 encounters for Alzheimer’s, 69 encounters for COPD, and 50 encounters for osteoporosis – a stark difference across all three illnesses..
As patients with well-managed chronic disease can be treated primarily in outpatient settings, and are less likely to require emergency and inpatient services, these findings highlight the higher disease burden for chronic disease patients in communities of color. But the power of these data points is in showing where targeted strategies to improve outcomes will do the most good.
Once a patient reaches the ER or requires inpatient care, the systemic disparity in care has already taken hold. For meaningful change to occur, health systems will have to not only observe these gaps, but put processes in place that will help to identify chronic disease in patients of color earlier and drive access that enables more proactive disease management through regular primary-care visits and medication optimization. It will not be easy, but with better data, the answers are closer than ever before.
To read our full research brief, click here.







