Data Challenges Can Limit Accurate Insights for Transgender Patients — But New Tools Can Help

Good data is one of the most powerful tools we have for improving health care and equity. Accurate and relevant insights can elucidate trends, quantify disparities, and pinpoint moments of opportunity for effective intervention. For communities that already struggle with visibility, good data is especially powerful and can mean the difference between a legislative bill being passed or not, the media covering a topic or not, and, ultimately, a patient receiving a life-changing treatment or not.
As datasets grow, though, so too does the number of errors and inaccuracies they contain. And in today’s interconnected, data-driven healthcare ecosystem, one misrepresentative record in a single database can proliferate into compounding errors, sending false signals that reverberate everywhere, from clinical trial data to value-based payment models.
One population that is disproportionately affected by these challenges is the transgender community. Errors can occur any time a patient changes an identifier, like name or gender, or changes payers. For example, two or more representations of an individual can be recorded as two separate people (called a “split”) after a name change. As the transgender community has a higher rate of changes to identifiers, the data that reflects this group can have, by default, lower fidelity. This can present challenges in research as well in accurately defining the on-the-ground realities experienced by transgender patients in their healthcare journeys.
Other data challenges can result from simple system or keystroke errors made by providers, legal changes in partnership status, or a lack of consistent standards in encryption software. Whatever the cause, the introduction of these types of errors into the system has the unfortunate effect of reducing the quality and trustworthiness of the insights derived from the underlying data. Errors typically become apparent in the tokenization process, where patient data is converted into de-identified patient codes. This is where data errors can be flagged and fixed, or missed or mishandled, going on to contribute to inaccurate insights.
Accurate data is important for moving the needle on change and providing robust evidence to advocacy groups working toward health equity to ensure the needs of these patients are met. Komodo Health has spent the last nine years refining the process for creating a de-identified patient database that addresses and intercepts these types of errors before they can enter our Healthcare Map. Because of our visibility across hundreds of payers and millions of providers, we’re able to trace a specific person through multiple representations of their identity by observing the overlapping behavior of multiple versions of an identity. This allows us to build a patient graph to surface and resolve errors like splits or collisions in the data. The process creates the foundation of our enterprise technology platform and gives our clients the world’s most robust insights into real-world healthcare experiences of patient populations large and small.
Komodo Health has emerged as a trusted source for delivering high-fidelity insights on trends in transgender healthcare, with some of our analyses featured in Reuters and the New York Times. For these analyses, we were able to overcome some of the identifier challenges by using multiple codes in the same healthcare visit to ensure accuracy. The latter, however, does not always occur, which can make transgender patients harder to pinpoint in the data and limit our understanding of the full patient journey.
We recently conducted an analysis of preventative screening rates among transgender patients using only traceable events, as qualifying the clinical encounter with the presence of two or more codes wasn't a confirmation measure that could be used. In part, this was to understand how those data challenges may influence the results of an analysis. More broadly, we wanted to see if and how screening rates changed over the past five years, given the increase in legislation targeting this community, and how these rates compare to the general population.
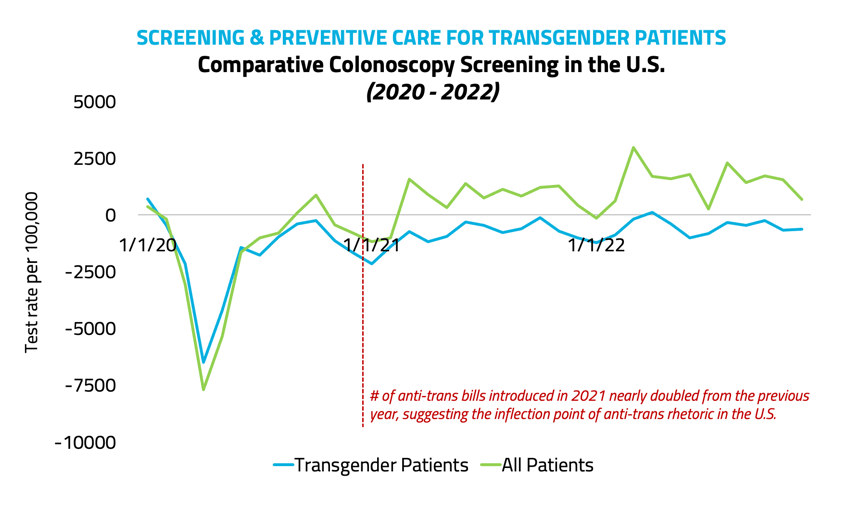
Looking at rates of mammograms, colonoscopies, and hemoglobin A1C blood sugar screenings, the numbers told us that mammograms and pap smears declined by just 1% and 2%, respectively in 2022, while colonoscopies and HbA1C screenings continued to trend upward. Compared to the general population, we also saw smaller declines in screenings among transgender patients in 2020, which is possibly reflective of the tokenization challenges, highlighting the difficulty in comprehensively analyzing independent events for this population. Given that, we suspect that transgender patient screenings are being under-captured. For analyses on single-code interactions, where transgender patients would typically show up in the data in the same way that cisgender patients do, there is still work to be done.
While these observations just scratch the surface of what’s needed for analyzing barriers to care and other systemic issues that could adversely affect health outcomes for the trans community, they do put a spotlight on the depth of data required to understand what’s really happening at the individual patient level. Barriers to care in this patient population are multifaceted, and removing them will require empowering advocates with robust and trustworthy statistics.
High-fidelity insights for populations with high rates of data complexity would not have been possible five years ago — when raw patient-count volume was emphasized above all, and we had not yet found ways to meaningfully address spits, collisions, and other data anomalies to ensure verifiable results. Volume alone is no longer the key to unlocking actionable insights for populations in need, especially in smaller ones, where every error carries more weight. These populations need high-fidelity, real-world patient journey data. Especially in trans healthcare, the approaches that advocates take to improve equity require maximum efficacy. Komodo's platform is here to help provide quality insights for next-generation evidence-building in high-need populations.
For more information about how linking data provides unprecedented insights from real-world evidence, check out  .
.
To see more articles like this, follow Komodo Health on Twitter, LinkedIn, or YouTube, and visit Insights on our website.







