Nearly 5% of Paxlovid Patients See COVID Rebound After 5 Days

At the onset of the COVID-19 pandemic, the primary focus for drug researchers and developers was finding a vaccine. The goal was twofold: 1) Prevent as many infections as possible, and 2) “de-fang” the virus so that when a breakthrough infection did occur, the resulting course of illness would be significantly less severe.
Thanks in large part to the urgency of the pandemic, multiple highly effective vaccines were brought to market in record time, and they have likely saved hundreds of thousands of lives already. Even still, COVID-19 continues to spread, which can leave vulnerable populations susceptible to eventual infection, with the potential to result in severe illness.
That explains pharmaceutical companies’ continued push to develop antiviral therapies, and why Pfizer’s Paxlovid has been viewed by drug makers and providers alike as a game changer. When taken within five days of developing COVID symptoms, the two-medication treatment inhibits the SARS-CoV-2 protein from replicating, which usually results in less severe disease.
For many, that has been the case, as Paxlovid has significantly reduced symptoms in individuals who are at risk of severe COVID – including older adults and those with underlying health conditions. However, an increasingly significant sample of patients that have taken Paxlovid have experienced “rebound cases,” where COVID-19 symptoms recurred after they completed treatment and experienced improvement in their symptoms. Komodo Health has dug into this issue using its Healthcare MapTM of real-world patient journeys and found that Nearly 5% of patients treated with Paxlovid experience a rebound in COVID diagnosis five or more days after being treated..png?width=900&name=Komodo_1200x800_Paxlovid_1in22_Blog%20(1).png)
Specifically, the Komodo Health analysis found over 100,000 patients treated with Paxlovid between December 2021 and April 2022. Of those, 4.5% experienced a recurrence of COVID diagnosis five or more days after initial treatment.
To put these numbers into the broader context of overall COVID-19 infection rates, the Komodo Health analysis also tracked the total number of patients who received at least one dose of a COVID-19 vaccine. All told, just 4.5% of patients who were partially or fully vaccinated received a subsequent COVID-19 diagnosis. The percentage of those with a subsequent Paxlovid prescription was 0.4%.
It’s worth noting some important limitations of this dataset, however. For one, the large-scale rollout of the COVID-19 vaccine through a combination of mass vaccination sites, employer-sponsored vaccination initiatives, and other formats has made it difficult to track the exact number of vaccines that have been administered. Komodo’s analysis is based primarily on vaccines that were administered with a corresponding health insurance claim. It is also important to note that the reported 4.5% of so-called “breakthrough cases,” or COVID-19 diagnoses following vaccination, could be artificially suppressed, thanks in large part to the widespread emergence of at-home testing.
Another interesting aspect to this story has been the availability of Paxlovid as COVID cases have increased and patients have scrambled to get prescriptions. Our analysis also tracked prescription volume by provider specialty to gauge which types of providers have been prescribing most frequently between December 2021 and April 2022.
Family Practice physicians wrote the most prescriptions, with 25%, followed by Internal Medicine (21%) and Nurse Practitioners (14%).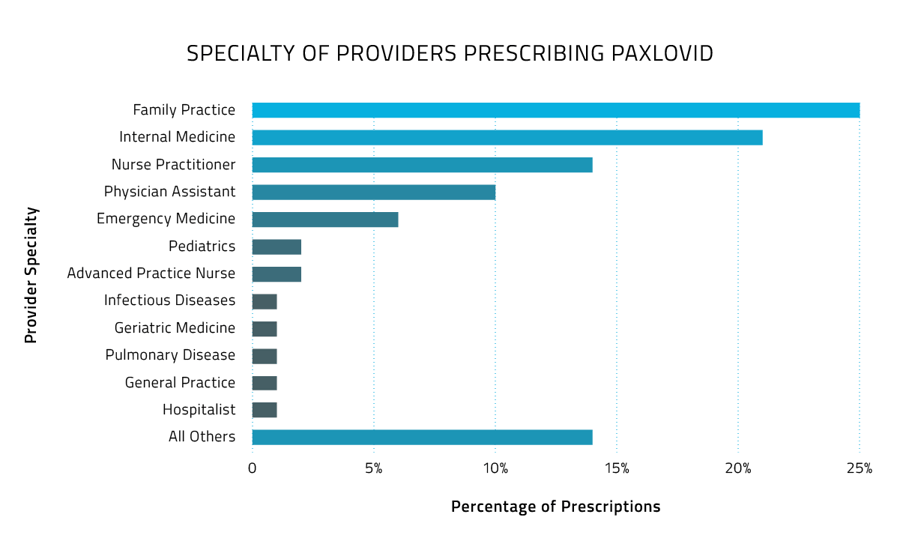 As COVID continues its march toward becoming endemic, Paxlovid will undoubtedly be a key tool at the disposal of frontline providers and their patients, just as other antivirals have helped against the annual ebbs and flows of influenza. As data becomes more robust on who is experiencing rebound cases, researchers may soon begin to understand why. Our hope is that the ongoing emergence of real-world evidence on the use of these types of therapies will help pave the way for increasingly mild COVID cases and better patient outcomes.
As COVID continues its march toward becoming endemic, Paxlovid will undoubtedly be a key tool at the disposal of frontline providers and their patients, just as other antivirals have helped against the annual ebbs and flows of influenza. As data becomes more robust on who is experiencing rebound cases, researchers may soon begin to understand why. Our hope is that the ongoing emergence of real-world evidence on the use of these types of therapies will help pave the way for increasingly mild COVID cases and better patient outcomes.
For more insights about the COVID-19 pandemic from Komodo Health, read our recent analysis on  .
.
To see more articles like this, follow Komodo Health on Twitter, LinkedIn, or YouTube, and visit Insights on our website.







