Insights Without a Code: How New Approaches Can Raise Visibility Into Ultra-Rare Diseases

For nearly 115 years, the International Classification of Diseases (or ICD) codes have been foundational to the healthcare industry’s ability to track, understand, and even exchange payment for medical diagnoses and care. Categorizing diseases and procedures, these codes are the shared language for payers, providers, and public health and Life Sciences organizations, ensuring clarity and consistency across patients. With nearly 70,000 clinical diagnostic codes, most diseases are captured. But what happens when a disease isn't represented?
Most rare diseases still don’t have a designated ICD-10 diagnosis code, and single codes are sometimes used for several distinct rare conditions. Roughly a quarter of ICD-10 codes match to more than one disease, and some codes match to many more. Q82.8, for example, the code for “other specified congenital malformations of skin,” was found to match to 22 rare diseases in a 2014 analysis. Without a specific code, gathering information about a disease is difficult. Risk factors, symptoms, and the nuances of a patient's journey get lost in the noise. These “codeless diseases” make patient identification, cohort generation, and clinical trial recruitment more difficult, leaving providers with poor visibility into case reports and the experiences of other rare disease patients, and higher barriers to the development of effective treatments and therapies. To prevent these patients from falling through the cracks, we need software that can easily circumvent coding limitations.
A Case Study: aHUS
Atypical hemolytic uremic syndrome (aHUS) is an example of a rare disease without an ICD-10 diagnosis code. aHUS affects around 1 in 500,000 people per year in the United States and is most often triggered by another medical event, such as an organ transplant or pregnancy atop a genetic predisposition. It affects kidney function and often results in dangerous blood clots that can restrict or block blood flow in the body, leading to serious health complications.
aHUS shares many similarities to other rare diseases, and has several treatment modalities that overlap with other conditions. It falls under the umbrella of the code for hemolytic uremic syndrome (HUS), of which about 90-95% of cases are typical HUS. However, HUS and aHUS are very different diseases, with different underlying causes and a different treatment protocol.
Using Prism to Create a Cohort of Hidden Patients
So how can we apply patient journey analytics to patient populations for which there is no specific ICD-10 diagnosis code? At Komodo Health™, we use our clinical expertise, our Healthcare Map™, and the universal cohort creator in our Prism tool to quickly build a snapshot of what a “typical” aHUS patient looks like.
To create an initial cohort of patients with the highest likelihood of having aHUS, we first identified the 3,266 patients with a diagnosis under the HUS code in 2019. Then, we selected out patients that had any history of causative factors in typical HUS, such as shigellosis, E. coli, and pneumonia, and applied aHUS-specific treatment codes to narrow the cohort to patients who had received one or more typical aHUS treatments (medications or procedures) within one year after their HUS diagnosis. What resulted was a complex cohort of 370 patients across the U.S. with a very high likelihood of having aHUS — created in minutes.
In other therapeutic areas, to pull in any missed patients, we might also check for standout factors in the cohort’s patient journey and extrapolate them to a more general cohort. In this example, there were no standout factors in the patient journey to apply.
What We Found: A Snapshot of aHUS Patients
We quickly learned that these 370 patients were under the care of 322 health care providers primarily in the specialties of nephrology/renal medicine, hematology and oncology, and critical care. Of these, 74% of patients had visited the emergency department in the year following their diagnosis, indicating potential opportunities to make improvements to early aHUS management. Common comorbidities in the patient group included acute kidney failure (82%) and anemia (79%), information that may help point to opportunities to identify candidates for prediagnostic screening or to ensure that the right tests are done at diagnosis.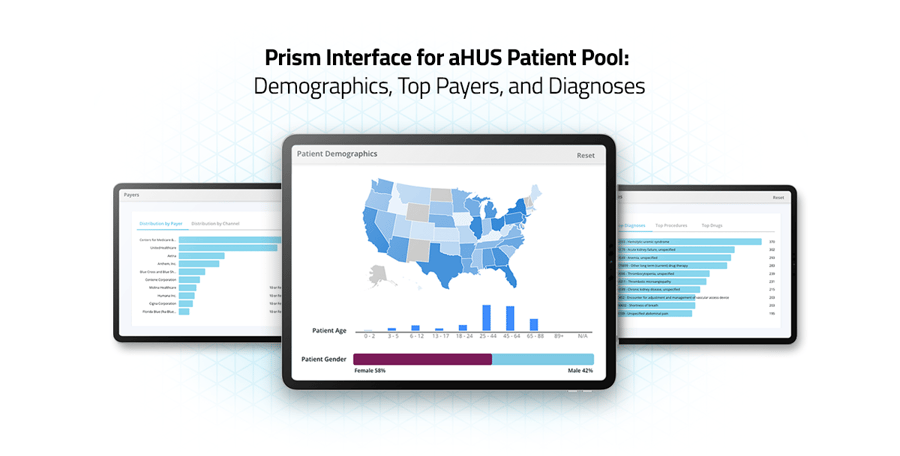 From here, we can dig deeper into many areas: estimate how many patients may be eligible for a new clinical trial, or learn about the patients’ providers in preparation for outreach with a new treatment option. We can also look at trends and deep insights into who these patients are, and the health journeys they’ve taken: their demographics, their symptoms, what type of testing they have undergone, the treatments they’ve received and when, the clinical events that preceded their diagnosis, and whether or not they’ve followed the most common treatment pathways. We can also see common misdiagnoses that patients have received before their diagnosis — an insight relevant for any specialists working in rare disease, where misdiagnoses are common.
From here, we can dig deeper into many areas: estimate how many patients may be eligible for a new clinical trial, or learn about the patients’ providers in preparation for outreach with a new treatment option. We can also look at trends and deep insights into who these patients are, and the health journeys they’ve taken: their demographics, their symptoms, what type of testing they have undergone, the treatments they’ve received and when, the clinical events that preceded their diagnosis, and whether or not they’ve followed the most common treatment pathways. We can also see common misdiagnoses that patients have received before their diagnosis — an insight relevant for any specialists working in rare disease, where misdiagnoses are common.
Looking Forward: New Possibilities for Rare Disease
So, what do we gain when we can identify population cohorts associated with a rare disease like aHUS, which has no ICD code? We can better study outcomes from different therapies; we can understand disease progression for sub-groups of the patient population; we can more easily identify clinical trial candidates.
Identifying, grouping, and analyzing patients with this level of granularity has historically been impossible without lengthy and costly efforts. Today, we can identify patients and patient cohorts for rare and orphan diseases, even where there is no existing ICD-10 diagnosis code. However, it still requires some advanced clinical knowledge and capabilities and an underlying data source that is comprehensive enough to combine multiple clinical signals in a meaningful way. Our Prism tool, which sits atop the Healthcare Map, can not only create the requisite patient cohort, but can also identify other critical moments along the patient journey. Ultimately, these types of analyses could help support healthcare and Life Sciences stakeholders to advance earlier diagnosis and reduce disease burden.
For more on our approaches to rare disease research, check out, “ ,” or read about
,” or read about  through our partnership with the Chan Zuckerberg Initiative.
through our partnership with the Chan Zuckerberg Initiative.
To see more articles like this, follow Komodo Health on Twitter, LinkedIn, or YouTube, and visit Insights on our website.







